I have not been on an aeroplane or done any travel outside the British Isles since before the pandemic. The reason is that I have been on a long road of recovery from a Covid-19 infection.
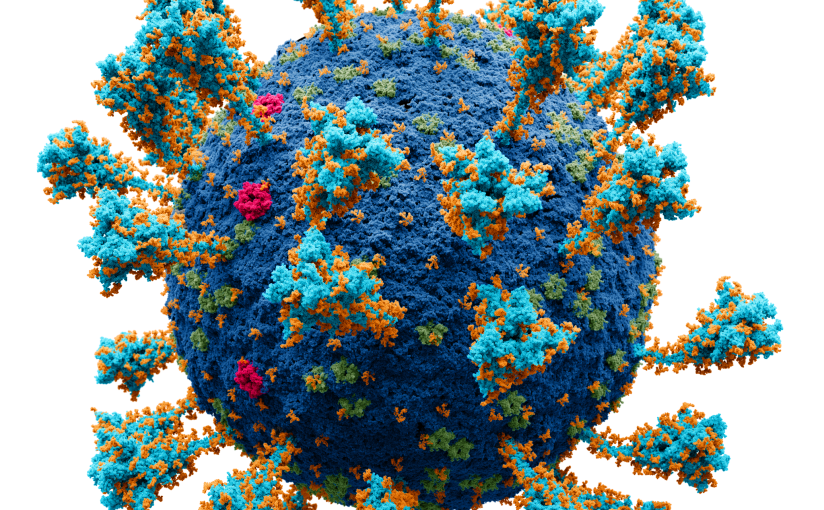
I contracted Covid (give it its full name: coronavirus SARS-CoV-2) in Aug 2022, my one and only infection, as far as I am aware. Although I am now largely recovered, it has taken about a year and a half to get back my strength.
I still have some after-effects, i.e. Long Covid, and I like to say that I am not the same man that I was before the Chinese stealth virus rewired my mind (!), but I am happy to report that I am much better, as much as one can ever be sure, that is, that this stealthy virus has finished with you!
The main symptoms of Long Covid usually include fatigue, breathlessness, headaches, chest pains, palpitations and dizziness, although there is not a widely accepted definition of this chronic illness, as this Royal Society website explains. I thought that it would be useful therefore, to briefly describe my own encounter with the syndrome and place it in the context of my own previous experiences of having another debilitating ailment: post-viral fatigue/ME.

As someone who has suffered from intermittent bouts of post-viral fatigue for much of my adult life, I was probably a sitting duck for Long Covid! Like many of us at the time however, I had a pretty cavalier attitude towards Covid when it first appeared. I remember thinking to myself: perhaps it would be a good idea to expose myself to the virus in order to build-up some immunity. The idea of herd immunity was doing the rounds, especially in government circles.
We were all very naïve about this virus, including prime ministers and health secretaries, and sadly many people have still not learnt how serious the symptoms can be, albeit for a relatively small proportion of the population. Nevertheless, according to the Office of National Statistics, that small proportion (three percent or more) constitute an estimated 2.0 million people in the UK experiencing self-reported Long Covid continuing for more than four weeks after the first coronavirus (COVID-19) infection
The Covid infection I experienced in Aug 2022 was not particularly severe, I have had worse bouts of flu in the past, but the after-effects were very debilitating. The main symptoms I suffered were chest pains, head-aches, insomnia, and bowel problems. I was also incredibly susceptible to cold and windy weather and went about dressed up for the Arctic, with long John’s and thermal vests, which made me sweat, of course. If I got too cold, I started to shiver and feel awful, and I had to take to my bed. Recovery usually took a day or so. I often piled on a ridiculous number of blankets to get warm again and I began calling these bouts ‘meltdowns‘.
“the variant of SARS-CoV-2 a person was first exposed to determines how well their immune system responds to different parts of the virus, and how protected they are against other variants.” (University of Cambridge Link)
This susceptibility to cold continued for at least a year, and I am still (18 months later) very cautious about going out in cold, windy weather. I also suffered ‘meltdowns’ if I overdid it in any way. Walking too fast or too far, for example. These symptoms of post-exertional fatigue were very similar to those I have had in the past during prolonged bouts of recovery from viruses: i.e. chronic fatigue syndrome. My experience of ME/CFS in the past always occurred as a result of a cold or flu virus, and I usually recovered after a month or three!😊.
Sensory overload: In the months following my Covid infection, I could not tolerate cold, hot sun, wind, or noise. Noisy situations would bring on a sort of brain fog, and cold and heat would precipitate ‘meltdowns’! But gradually, things did improve. There seems to be a general consensus that it takes about 18 months to recover from Long Covid; but this is very much an average, and many people will take much longer, or much shorter. It all depends on the severity of the initial infection and your own genetics (=immune system).
Looking back: The first time I got ME, as I call it, I was in my 30’s, but when I look back over my life, I have had periods of fatigue which were strange and difficult to link to obvious episodes of illness. For example, during the run-up to my A levels, I found it impossible to revise. I got sick and felt ill as soon as I looked at my notes!
This is why some doctors, not so many now, thought that ME was ‘all in the mind’. In reality it is in the mind AND the body, and strangely enough, in the gut!
In the end, I took all of my A levels without having done any revision at all! Luckily, I was enough of a swat to pass them all satisfactorily, based on what I had done before. Fortunately, this lethargy did not happen again, for example, when I took the exams for my degree, but I did know a fellow student who got ill and simply was not able to study anymore.
The symptoms of Long Covid (LC) and ME/CFS are both mind/body illnesses. In other words, they affect both the body and mind of the patient. This led many doctors to come to the conclusion that they were dealing with depression, and many medics prescribed antidepressants for ME. These drugs can, however, help, but that does not mean that ME/CFS is just in the mind!
In my experience, some people get ‘stuck’ in their illnesses: LC or ME. It can be difficult to extricate yourself from the malaise.
One has to find a way out of the illness, and the route may vary for each patient or sufferer of LC or ME/CFS. I am grouping these illness together because they can be very similar, but in my experience, every post-viral episode is different, even in the same person. This is because viruses differ and evolve, and our immune systems are also learning and changing throughout life.
When I first got a severe bout of ME in my thirties (I am now 69) it took a long time to get well (4-6 months). One tends to get a bit stuck and there seems to be no way to get back to a normal state of mind and health. My own breakthrough came in the form of a meditation tape which a chiropractor gave me. This enabled be to really relax (on the floor) every day and focus on my breathing. I also tried to eat well and gradually built up my strength by gentle walking.
Exercise is important, but don’t overdo it. Keep within your limits, if you can find them.
I got very little support from the medical profession. I remember one doctor saying: “Some of my patients get sick every winter and do not recover until the spring.” Yes, I thought, but do you have anything to offer them in the way of advice or treatments?
Maybe I’m being too harsh? I got very upset when my mother’s cat died and the vet couldn’t help. “Do something,” I shouted! “It’s dead,” said the vet. Useless bugger I thought!
Gut feelings: I remember telling another doctor that I thought the root cause of ME lay in the gut. He looked at me as though I was an idiot. In the gut? This was about 1990; we now know that disruption of the gut microbiota may well be a contributing factor in ME/CFS, and there are positive effects of probiotic therapy. The gut–brain axis plays a really important role in regulating physical and mental health.
“Between 70 and 80 per cent of immune cells are in the gut, where they are constantly communicating with microbes. This crosstalk helps fight disease, strengthen immune responses and regulate inflammation, our body’s first line of defence against infection” (New Scientist 3 October 2023)
“Long Covid has taken all that I took for granted as being stable in my life, lifted it up, shaken it, put it down again and left me to make sense of what was left, like one of those snow globes, except not so pretty.” (Gahan, 2023)
My experiences with the medical profession with Long Covid were not much better than with ME. I expect there are good specialists, certainly now, but accessing them is not always easy. The NHS tackle each symptom separately, and understandably, go down well-trodden pathways to establish whether there are any severe underlying problems. So, when I presented myself in A&E with chest pains, I got X-rayed (there was nothing to be seen) and sent up to be examined for heart problems. I came away from that first session, having been prescribed medication for angina. I knew I didn’t have angina, because I could walk up long flights of stairs without problems (other than fatigue). I subsequently had an ECG and an echocardiogram and finally saw a consultant heart specialist. There was nothing wrong with my heart!
We now know that traditional chest X-ray can reveal only so much and cannot distinguish compromised lung function resulting from the novel coronavirus. A novel scanning method using xenon gas was developed by scientists at the University of Sheffield, to detect lung abnormalities not identified by routine scans.
“Although respiratory symptoms belong to the most common symptoms in long COVID patients, this is not necessarily linked to radiologically detectable lung damage.“ (A Systematic Review of Chest Imaging Findings in Long COVID Patients).
On another occasion, visiting a GP practice for chest pains, I was given antibiotics. I somehow knew that I did not have an infection. The rattly sounds of my chest were a Long Covid symptom. Similarly, with headaches, no one seemed to have a clue. I remember one consultant saying to me: “after the (viral) illness is over, the body clears itself of viroids; there are none left in the body”. Wrong, wrong, wrong! Even I knew that this was not the case. Were they not reading the literature?
Viral persistence:
“There is ample evidence for persistence of SARS-CoV-2 viral RNA and proteins in several tissues, including respiratory tract, GI tract, olfactory mucosa, and the central nervous system” (eLife. 2023; 12: e86015, doi: 10.7554/eLife.86015).
“Long COVID could occur by various mechanisms, including viral persistence, SARS-CoV-2 superantigen–mediated activation of the immune system, and autoimmunity.” (Nature Medicine 28, 879–882 (2022) https://www.nature.com/articles/s41591-022-01766-7)

Hypothesized mechanisms of long COVID pathogenesis. There are several hypothesized mechanisms for long COVID pathogenesis, including immune dysregulation, microbiota disruption, autoimmunity, clotting and endothelial abnormality, and dysfunctional neurological signaling. EBV, Epstein–Barr virus; HHV-6, human herpesvirus 6; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2. Credit: Nature Reviews Microbiology (2023). DOI: 10.1038/s41579-022-00846-2
Fatigue: Fatigue is not the same as tiredness. You just don’t have the energy to do things, even if you have had a good rest. Brains get fatigued, and bodies get fatigued. Why we don’t we bounce back after a good rest, after contracting a virus, I don’t know. There must be a physical cause. But the changes must be very tiny, at the cellular level, and difficult to detect, I suppose. Medicine does not usually operate at that level. But research does: it just needs studying, and because more people have Long Covid than have ME, the Covid pandemic may lead to a better understanding of these autoimmune diseases. Maybe!
Symptoms
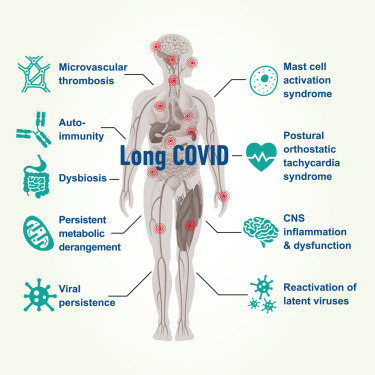
Although, LC symptoms have been likened to a ‘lucky dip’ (unlucky dip rather!), where the particular constellation of symptoms varies from person to person, recent research has identified three main clusters, or types of symptoms:
i) a cardio-respiratory cluster of symptoms,
ii) a central neurological cluster, and
iii) a multi-organ systemic inflammatory cluster (Canas et al., 2023).
“different profiles of post-COVID-19 condition, characterised by differing symptom combinations, durations, and functional outcomes” (Canas et al., 2023).
In plain language, this study found that the largest group of LC sufferers experienced neurological symptoms such as fatigue, brain-fog and headaches, whilst a second group experienced respiratory symptoms including chest pain and severe shortness of breath, possibly as a result of lung damage. The third group was made up of people who experienced a diverse range of symptoms, including heart palpitations, muscle ache, and changes in skin and hair.
In my own case, the progression of the post-viral Long Covid symptoms followed a rough pattern of chest, brain (headaches and tinnitus), and gut problems.
Taste and smell loss are common symptoms of Covid-19 that may emerge and persist long after initial infection, but fortunately I never lost my sense of smell.
Brain fog or brain fatigue
People with symptoms for 12 weeks or more fell into three main groups based on the types of symptoms they were experiencing. The largest group was characterised by a cluster of neurological symptoms such as fatigue, brain-fog and headache and was the most common subtype among alpha and delta variants. A second group experienced respiratory symptoms, including chest pain and severe shortness of breath, which could point to lung damage. This was the largest cluster in the wild-type period when the population was unvaccinated. Finally, there were some people who experienced a diverse range of symptoms, including heart palpitations, muscle ache and pain, and changes in skin and hair. (Three types of long-COVID for people experiencing symptoms for 12 weeks or more)
Post-exertional fatigue or crashing out! “Boom and bust”—you feel great, do a little bit more than usual, and come crashing down the next day. (Link 3)
Psychological effects – avoid noise and stimulus – feel like I have been ‘rewired’!
Flare-ups: what’s going on? It may be to do with MAST cells.
In the long COVID-19, a persistent inflammatory state will activate specific mast cell genes that will cause an abnormal mast cell activation control. (Sumantri & Rengganis, 2023)
COVID-19 infection could lead to exaggeration of existing undiagnosed mast cell activation syndrome, or could activate normal mast cells owing to the persistence of viral particles. (Arun et al., 2022)
Progress: I liken recovery from LC or ME to an expanding balloon (below). You gradually get your energy and brain power back. But whether you get back to where you were is debatable!

Pace yourself and don’t overdo it. Learn how to relax. Try to listen to soothing music and sink into the sofa. Really let go. Let that diaphragm relax. Clear the mind. Think nice thoughts. Eat good food.
Most people with Long Covid (as with ME) sometimes come to the conclusion that they are on their own and have to try and find their own way out of their post-viral malaise. If they can; but there are resources out there if you reach out. Things have improved somewhat after the Covid epidemic: many hospitals have LC clinics, and the NHS introduced a Living with Long Covid App. It’s helpful, but for me, it didn’t capture the subtleties of the illness.
Treatments: Don’t get too excited, because there aren’t any! As far as I am aware, there are no treatments being routinely offered by the NHS for Long Covid in the UK. However, there is plenty of good advice now, recovery programmes and Long Covid clinics. See here.
In my experience, the best treatments are rest and relaxation. Plus good diet; healthy foods. However, not everyone has the luxury of putting their life on hold for a while whilst they recover. It must be particularly hard for mothers with children to look after. And for some unknown reason, women seem to suffer more from these diseases than men.
Slow down and pace yourself: “There are no limits!” Spouts an online athletics coach. “Limitations are all in your mind”. Not if you have LC they’re not! There are well-defined limits to your physical and mental capacities and if you transgress them, you pay a price. Overdo your exercise programme and you will wind up back in bed, feeling awful for an undefined recovery period.
During the early stages – i.e. the first couple of months of my own LC journey, I felt sicker than I have ever felt before, especially during the bouts when I ‘crashed out’. It was much worse than the infective stage of the virus, worse than the worst bout of flu I can remember. But, I knew that it was temporary; I just keep taking paracetamols and sucking on sugar-free sweets (it seemed to help!), and the discomfort eventually receded. Until the next time I overdid it!
But, my long Covid was fairly mild compared to some people.
With time, I recovered, as most people do, I think. Hopefully, this blog, and the links below, might help a few people struggling with these symptoms.
Links
https://www.gov.uk/government/news/new-research-into-treatment-and-diagnosis-of-long-covid
https://magazine.alumni.ncsu.edu/2022/the-long-haul/
https://www.kcl.ac.uk/news/three-types-long-covid-people-experiencing-symptoms-12-weeks
https://www.ft.com/content/ff63cd68-7281-4340-b1b6-5db3d891eaff
Paul Garner: Covid-19 and fatigue—a game of snakes and ladders
BBC News – Long Covid: Three years and no magic bullet
https://www.bbc.co.uk/news/uk-scotland-65058119
References
Arun S, Storan A, Myers B. Mast cell activation syndrome and the link with long COVID. Br J Hosp Med (Lond). 2022 Jul 2;83(7):1-10. doi: 10.12968/hmed.2022.0123. Epub 2022 Jul 26. PMID: 35938771.
Astin, R., Banerjee, A., Baker, M. R., Dani, M., Ford, E., Hull, J. H., … & Hall, C. N. (2023). Long COVID: mechanisms, risk factors and recovery. Experimental physiology, 108(1), 12-27.
Burges Watson, D. L., Campbell, M., Hopkins, C., Smith, B., Kelly, C., & Deary, V. (2021). Altered smell and taste: Anosmia, parosmia and the impact of long Covid-19. PloS one, 16(9), e0256998.
Canas, L. S., Molteni, E., Deng, J., Sudre, C. H., Murray, B., Kerfoot, E., … & Modat, M. (2023). Profiling post-COVID-19 condition across different variants of SARS-CoV-2: a prospective longitudinal study in unvaccinated wild-type, unvaccinated alpha-variant, and vaccinated delta-variant populations. The Lancet Digital Health.
Callard, F., & Perego, E. (2021). How and why patients made Long Covid. Social science & medicine, 268, 113426.
Décary, S.; Gaboury, I.; Poirier, S.; Garcia, C.; Simpson, S.; Bull, M.; Brown, D.; Daigle, F. Humility and Acceptance: Working Within Our Limits With Long COVID and Myalgic Encephalomyelitis/Chronic Fatigue Syndrome. J. Orthop. Sports Phys. Ther. 2021, 51, 197–200. https://pubmed.ncbi.nlm.nih.gov/33930983/
Davis, H.E., McCorkell, L., Vogel, J.M. et al. Long COVID: major findings, mechanisms and recommendations. Nat Rev Microbiol 21, 133–146 (2023). https://doi.org/10.1038/s41579-022-00846-2
Gahan, Dr Luch (2023). Breaking free from Long Covid. Reclaiming Life and the Things that Matter. Jessica Kingsley Publishers. https://www.nature.com/articles/s41579-022-00846-2#citeas
Raveendran, A. V., Jayadevan, R., & Sashidharan, S. (2021). Long COVID: an overview. Diabetes & Metabolic Syndrome: Clinical Research & Reviews, 15(3), 869-875.
Scurati R, Papini N, Giussani P, Alberti G, Tringali C. The Challenge of Long COVID-19 Management: From Disease Molecular Hallmarks to the Proposal of Exercise as Therapy. International Journal of Molecular Sciences. 2022; 23(20):12311. https://doi.org/10.3390/ijms232012311
Sumantri S, Rengganis I. Immunological dysfunction and mast cell activation syndrome in long COVID. Asia Pac Allergy. 2023 Mar;13(1):50-53. doi: 10.5415/apallergy.0000000000000022. Epub 2023 Apr 28. PMID: 37389095; PMCID: PMC10166245.
Wilks, S H et al: ‘Mapping SARS-CoV-2 antigenic relationships and serological responses.’ Science, October 2023. DOI: 10.1126/science.adj0070